A Patient with Advanced Metastatic Prostate Cancer
PSMA (Pluvicto) Therapy.

Case Study
Over subsequent years his PSA remained less than 1 and imaging work up with CT continued to show stable skeletal sclerotic lesions. In October 2023 the patient reported increasing lower back pain. PSA increased to 1.04 and in November 2023 it increased to 1.15.
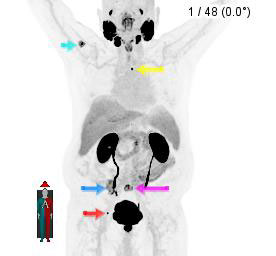

Therefore, a PSMA PET/CT was ordered, which showed (figure 1) several skeletal metastatic lesions, including the one at the site of patient’s lower back pain (figure 1, purple arrow). This patient with castrate resistant metastatic prostate cancer therefore underwent four cycles of 177Lu-PSMA-617 treatments December 2024 through April 2024. The patient reported complete resolution of lower back pain.
A repeat PET/CT (figure 2) showed considerable interval improvement in skeletal metastatic lesions, including the site of lower back pain.
Taking advantage of unique quantitative assessment of PET/CT we performed tumor burden assessment before and after 177Lu-PSMA-617 treatment cycles (figure 3), which showed 85% decrease in his total body tumor burden after 4 cycles of Lu-177 PSMA therapy.
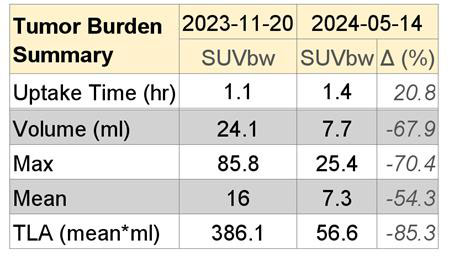
PSA levels went down from 1.15 ng/mL before initiation of 177Lu-PSMA-617 to 0.48 after four cycles of therapy. Since the most recent PSMA PET/CT still shows small volume of residual PSMA-avid skeletal metastatic lesions our plan is to continue remaining 2 cycles of therapy.
Discussion
References
Dr. Munir Ghesani, MD, FACNM, FACR, FSNMMI

Dr. Ghesani has more than 200 publications in peer-reviewed journals and is the Editor-in-Chief of a three-part book on nuclear medicine and molecular imaging. He has given more than 150 presentations at regional, national, and international conferences.
